8th December 2023
67 Sai Likhitha
Thursday, 7 December 2023
Osce questions and learning points.
Wednesday, 6 December 2023
76 yr old female with pedal edema.
6th December 2023
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan.
Date of admission - 6th December 2023
A 76 year old lady home maker by occupation resident of nalgonda came to opd with chief complaints of
Pedal edema and shortness of breath since 4 days.
Decreased urine output since 4 days.
History of present illness:
She was apparently asymptomatic 1 month back then developed loss of appetite, indigestion, nausea and vomitings since 1 month for which she was taken to hospital and found to have raised urea and creatinine levels and was suggested to get dialysis done.
she presented with bilateral pedal edema pitting type extending upto the knee since 4 days.
Shortness of breath grade(1-2) since 4 days.
No history of chest pain and palpitations.
No history of burning micturition.
Daily routine before the onset of disease:
wakes up at 6:00 am.
Does all the household works like cooking, and cleaning utensils and tailoring work.
1-2 pm - eats lunch, sleeps after having lunch.
wakes up at around 4:00 pm does some stitching work or watches Tv.
Dinner around 8pm and sleeps after dinner.
Past history:
Known case of hypertension since 4 years and on medication clinod-t (clinidipine 10mg and telmisartan 40 mg).
Not a known case of DM, asthma, TB, epilepsy, CAD, CVD and thyroid diseases.
Personal history:
Diet :mixed
Appetite: decreased
Bowel and bladder movements regular
Sleep: adequate
No allergies and addictions
Family history: not significant
General examination:
Patient is conscious, coherent and cooperative.
Well oriented to time and place.
Moderately built and nourished.
Pallor- absent
Icterus - absent
No clubbing, cyanosis and lymphadenopathy.
Pedal edema- present
Temp: 98.2 f
Bp: 120/80mm hg
PR: 88 bpm
RR: 16cpm
Systemic examination:
CVS:s1s2+,no murmur
RS:BAE+,no added sounds
P/A:
Inspection: Shape of abdomen- slightly distended.
Position of umbilicus: central and inverted
No scars and sinuses are present
All quadrants are moving equally with respiration
Palpation:No tenderness
No organomegaly
Auscultation:
Bowel sounds heard
CNS: NFD
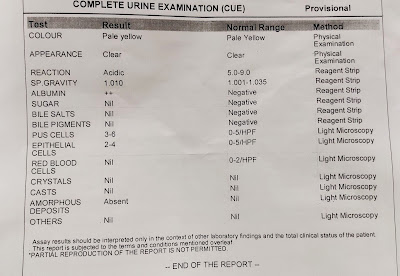
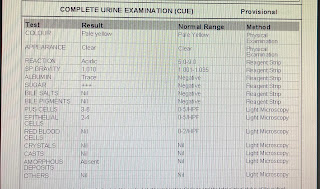
Investigations:
ECG:
Provisional diagnosis - chronic kidney disease on mhd.
Treatment given-
Wednesday, 29 November 2023
Wednesday, 19 July 2023
Thursday, 8 June 2023
Personal practical patient experience.
I'm K. Sai likhitha a medical student from India. Here in this blog i share my personal learning experience in medicine department beginning from my first patient practical interaction.
This elog has been created after taking the consent from the patient and their relatives. Links to some of the logged case reports are attached along with my personal patient experience and learning outcome from that particular case.
My experience with the case based blended ecosystem in medicine department has been very unique and transitional with time. Initially when i have seen our professors and interns discussing the cases through an online call during my second year of MBBS, i was very enthusiastic and interested but I have no idea about anything at that time. After a couple of similar online calls, my eagerness and interest has started sloping down and the only thing i have learnt during that time was to get aware of most of the terminology. It was almost more than one Android half year( due to covid) after joining in the first year of MBBS i have seen something like this and it really felt like the actual medicine training is gonna start from now. And from then it took a few more months to practically see the patients personally in the wards and talk to them.
First personal patient encounter
Link to the case: https://www.blogger.com/blog/post/edit/6532713601891436629/4849626673101142178
This is the case of a 34 year old female with recurrent vomitings since 6 months. Initially i was surprised that why does the vomiting didn't bother her at all since 6 months, eventually after seeing more patients i registered that pain is the ultimate thing that brings a person to the clinic. Many patients are concerned only when the symptoms are troubling their daily routine until then they don't want to visit the hospital. This patient even though she had vomitings since 6 months she came to hospital because the frequency of vomiting has increased and she could not perform her work due to weakness.
She was very thin built and on examination pallor was present. Her blood pressure was 110/60 mm hg. The provisional diagnosis was acute hypertension secondary to dehydration and vomitings.
This helped me improving my history taking skills and communication with the patients. I have also learned how the dehydration due to vomitings can cause the secondary hypertension with its effects on cardiac and renal systems.
Wednesday, 7 June 2023
50 yr old male with fever and cough with sputum.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan.
History of presenting illness:
Fever since 7-days high grade-not associated with chills and rigor, evening rise + Associated with sweating
Cough since 7- days associated with less amount of sputum, mucoid. blood tinged aggravated on changing position from lying down to sitting position, no reliving factors
SOB grade - I MMRC -: 7 days more associated with cough, relieved on rest not associated with wheeze
NO H/O similar complaints in the past
No past H/O TB, loss of appetite, loss of weight
K/C/O: Dm+ since 2years
N/K/C/O HTN,CAD ,Br Asthma ,epilepsy
H/o RTA 1 1/2 year back
Fracture of neck of femur with dynamic hip screw surgery done in outside Hospital.Immobilisation 1 month to 1-1/2 year back
- H/o -electrocution
4-years back - Burns both hands
PERSONAL HISTORY
Patient is Binge Alcoholic and Smokes 18 cigarettes in a day later he started smoking Bedi Suttas(high tobacco cigar) in day.
Patient attendant said that their neighbour has TB ( who is son in law of him )
And Patient visits weekly 4 times to his home & spend with him approximately 1-hour a day
Patient started to have fever since 10 days at night time with burning sensation all over the body
Patient started to have unbearable pain at lower back during cough .and always needed help from attendants to hold his back during coughing.
PAST HISTORY
K/c/o DM since 2 years was diagnosed during his RTA treatment and is on regular Glimiperide 1mg &Metformin 500mg medication since then.
He has no history of hypertension, diabetes ,asthma, epilepsy, tuberculosis.
GENERAL EXAMINATION
Patient is conscious, cooperative ,coherent and oriented with time , place , date.
Slightly pallor,
No icterus, cyanosis, clubbing, lymphadenopathy, edema was noted
Osce questions and learning points.
8th December 2023 Osce questions: 1) Hypertension causing chronic kidney disease vs chronic kidney disease leading to hypertension? Chron...
-
8th December 2023 Osce questions: 1) Hypertension causing chronic kidney disease vs chronic kidney disease leading to hypertension? Chron...
-
6th December 2023 This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians ...
-
1st September 2022 This is online E log book to discuss our patient’s de-identified health data. Here we discuss our individual patient’s pr...